Difference between revisions of "IPLab:Lab 6:Hashimoto's Thyroiditis"
Seung Park (talk | contribs) |
Seung Park (talk | contribs) |
||
| (2 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
== Clinical Summary == | == Clinical Summary == | ||
| − | This was a 49-year-old woman who complained during her yearly physical examination of tiredness and difficulty concentrating. She attributed these symptoms to stress at work. She had gained weight over the last year and despite warm weather, she felt chilled without a sweater. Family history was significant for hypothyroidism in her mother and older sister. On physical examination she had a pulse of 58 bpm and a blood pressure of 138/88 mm Hg. Examination of her neck disclosed a small thyroid gland with a palpable pyramidal lobe and a firm, bosselated texture. Serum taken at this time demonstrated a total T4 of 7.0 mcg/dL and a TSH of 22.0 mcIU/ml. In addition, antithyroglobulin antibodies were positive at 1 | + | This was a 49-year-old woman who complained during her yearly physical examination of tiredness and difficulty concentrating. She attributed these symptoms to stress at work. She had gained weight over the last year and despite warm weather, she felt chilled without a sweater. Family history was significant for hypothyroidism in her mother and older sister. On physical examination she had a pulse of 58 bpm and a blood pressure of 138/88 mm Hg. Examination of her neck disclosed a small thyroid gland with a palpable pyramidal lobe and a firm, bosselated texture. Serum taken at this time demonstrated a total T4 of 7.0 mcg/dL and a TSH of 22.0 mcIU/ml. In addition, antithyroglobulin antibodies were positive at 1 to 640 and antimicrosomal antibodies were positive at 1 to 5120. These results supported the clinical impression of hypothyroidism; also, the texture of her thyroid gland and a positive family history suggested an autoimmune etiological factor. She was referred to an endocrinologist for further evaluation; however, before beginning treatment she died suddenly from a ruptured berry aneurysm of the middle cerebral artery. |
== Autopsy Findings == | == Autopsy Findings == | ||
| Line 17: | Line 17: | ||
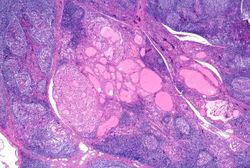
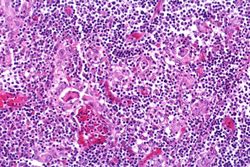
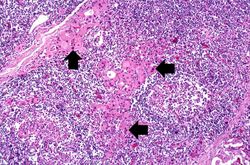
File:IPLab6Hashimoto9.jpg|This high-power photomicrograph shows more clearly the lymphocytes and plasma cells surrounding the thyroid gland epithelium. Large, eosinophilic, degenerating thyroid gland cells (Hurthle cells) can be seen in this section (arrows). | File:IPLab6Hashimoto9.jpg|This high-power photomicrograph shows more clearly the lymphocytes and plasma cells surrounding the thyroid gland epithelium. Large, eosinophilic, degenerating thyroid gland cells (Hurthle cells) can be seen in this section (arrows). | ||
</gallery> | </gallery> | ||
| + | |||
| + | == Virtual Microscopy == | ||
| + | <peir-vm>IPLab6Hashimoto</peir-vm> | ||
== Study Questions == | == Study Questions == | ||
| Line 35: | Line 38: | ||
=== Images === | === Images === | ||
| − | * [ | + | * [{{SERVER}}/library/index.php?/tags/15-endocrine/140-thyroid/141-lymphocytic_thyroiditis PEIR Digital Library: Lymphocytic Thyroiditis Images] |
* [http://library.med.utah.edu/WebPath/ENDOHTML/ENDOIDX.html WebPath: Endocrine Pathology] | * [http://library.med.utah.edu/WebPath/ENDOHTML/ENDOIDX.html WebPath: Endocrine Pathology] | ||
Latest revision as of 16:17, 3 January 2014
Contents
Clinical Summary[edit]
This was a 49-year-old woman who complained during her yearly physical examination of tiredness and difficulty concentrating. She attributed these symptoms to stress at work. She had gained weight over the last year and despite warm weather, she felt chilled without a sweater. Family history was significant for hypothyroidism in her mother and older sister. On physical examination she had a pulse of 58 bpm and a blood pressure of 138/88 mm Hg. Examination of her neck disclosed a small thyroid gland with a palpable pyramidal lobe and a firm, bosselated texture. Serum taken at this time demonstrated a total T4 of 7.0 mcg/dL and a TSH of 22.0 mcIU/ml. In addition, antithyroglobulin antibodies were positive at 1 to 640 and antimicrosomal antibodies were positive at 1 to 5120. These results supported the clinical impression of hypothyroidism; also, the texture of her thyroid gland and a positive family history suggested an autoimmune etiological factor. She was referred to an endocrinologist for further evaluation; however, before beginning treatment she died suddenly from a ruptured berry aneurysm of the middle cerebral artery.
Autopsy Findings[edit]
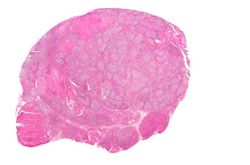
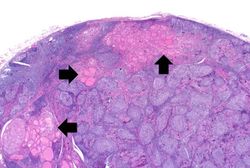
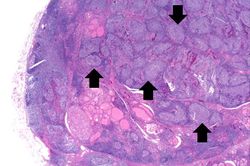
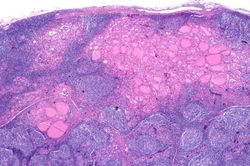
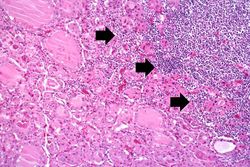
At autopsy, significant subarachnoid hemorrhage from the ruptured berry aneurysm was documented. In addition, the thyroid gland was mildly enlarged and firm. On cut section the tissue was slightly pale.
Images[edit]
Virtual Microscopy[edit]
Study Questions[edit]
Additional Resources[edit]
Reference[edit]
- eMedicine Medical Library: Hashimoto Thyroiditis
- eMedicine Medical Library: Hypothyroidism
- Merck Manual: Overview of Thyroid Function
- Merck Manual: Hashimoto's Thyroiditis
- Merck Manual: Hypothyroidism
Journal Articles[edit]
- Agrawal P, Ogilvy-Stuart A, Lees C. Intrauterine diagnosis and management of congenital goitrous hypothyroidism. Ultrasound Obstet Gynecol 2002 May;19(5):501-5.
Images[edit]
Related IPLab Cases[edit]
A normal pulse rate is 60 to 100 bpm.
A normal blood pressure reading would be 120/80 mm Hg.
Bosselated means covered with rounded protuberances.
A normal T4 level is 4 to 11 mcg/dL.
A normal TSH level is 0.32 to 5.00 mcIU/dL.
Antithyroglobulin antibodies are autoimmune antibodies directed against thyroglobulin. Over half of all patients with Hashimotos thyroiditis have positive titers, although they are also found in other types of thyroiditis.
A normal antithyroglobulin antibody titer would be less than 1 to 10.
Antimicrosomal antibodies are autoimmune antibodies directed at the thyroid gland. They are seen in almost all patients with Hashimotos thyroiditis.
A normal antimicrosomal antibody titer would be less than 1 to 100.
Autoimmune disorders involve an immune response directed at the host's own cells.
A berry aneurysm is a small saccular arterial aneurysm usually found at a vessel junction in the circle of Willis. These aneurysms frequently rupture, causing a subarachnoid hemorrhage.