Difference between revisions of "IPLab:Lab 13:Hyaline Membrane Disease"
Seung Park (talk | contribs) |
Seung Park (talk | contribs) (→Liver) |
||
| (10 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
== Clinical Summary == | == Clinical Summary == | ||
| − | This 28-hour-old white male was the product of an uncomplicated vaginal delivery by a G1 24-year-old mother whose pregnancy had also been uncomplicated. The infant was born pre-term at 36 weeks gestation and was appropriate for gestational age, weighing 2550 grams. Three hours after birth, the infant developed cyanosis and required 40% oxygen to maintain a pink color. Because of a worsening respiratory distress syndrome, the infant (1 day old) was transferred to a tertiary care hospital with a neonatal intensive care unit. Following the transfer, the respiratory distress progressed and the admitting arterial blood gases were pH 7.31, | + | This 28-hour-old white male was the product of an uncomplicated vaginal delivery by a G1 24-year-old mother whose pregnancy had also been uncomplicated. The infant was born pre-term at 36 weeks gestation and was appropriate for gestational age, weighing 2550 grams. Three hours after birth, the infant developed cyanosis and required 40% oxygen to maintain a pink color. Because of a worsening respiratory distress syndrome, the infant (1 day old) was transferred to a tertiary care hospital with a neonatal intensive care unit. Following the transfer, the respiratory distress progressed and the admitting arterial blood gases were pH 7.31, PaCO2 35, and PaO2 35. The condition of the patient continued to deteriorate despite therapy, and he became "shocky" with efforts to increase blood volume. He developed a persistent bradycardia and died about 4 hours after admission. |
== Autopsy Findings == | == Autopsy Findings == | ||
| Line 17: | Line 17: | ||
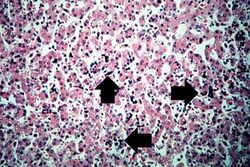
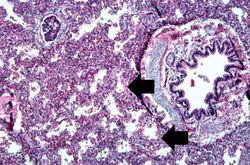
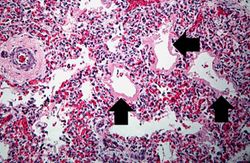
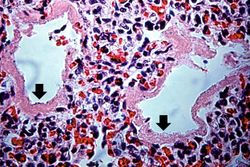
File:IPLab13Hyaline9.jpg|This higher-power photomicrograph shows more clearly the hyaline membranes (arrows) and the congestion in the interstitium. | File:IPLab13Hyaline9.jpg|This higher-power photomicrograph shows more clearly the hyaline membranes (arrows) and the congestion in the interstitium. | ||
</gallery> | </gallery> | ||
| + | |||
| + | == Virtual Microscopy == | ||
| + | === Liver === | ||
| + | <peir-vm>IPLab13Hyaline_liver</peir-vm> | ||
| + | |||
| + | === Lung === | ||
| + | <peir-vm>IPLab13Hyaline_Lung</peir-vm> | ||
| + | |||
| + | == Study Questions == | ||
| + | * <spoiler text="What causes Respiratory Distress Syndrome (RDS), or Hyaline Membrane Disease (HMD) as it is described in this case?">Most cases of respiratory distress syndrome (RDS) or hyaline membrane disease are idiopathic (the cause is unknown). | ||
| + | |||
| + | Known contributory factors include: | ||
| + | # over-administration of sedatives to the mother during delivery leading to respiratory depression in the infant; | ||
| + | # failure of the infant's central respiratory centers due to brain injury; | ||
| + | # reduced respiratory ability of the infant secondary to lung and skeletal muscle immaturity; | ||
| + | # physical obstruction of ventilation caused by the aspiration of blood clot and amniotic fluid during birth, and | ||
| + | # partial asphyxiation of the infant resulting from restrictive coils of umbilical cord wrapped around the infant's neck.</spoiler> | ||
| + | * <spoiler text="What factors play important roles in the pathogenesis of this syndrome?">Deficiency of pulmonary surfactant is the basic defect in respiratory distress syndrome. | ||
| + | |||
| + | Surfactant reduces surface tension within the alveoli so that less pressure is required to hold alveoli open. Surfactant also maintains alveolar expansion by varying surface tension with alveolar size, which helps keep the alveoli open and reduces the inspiratory effort needed to expand the lung. With a deficiency of surfactant, the lungs collapse with each successive breath, so the infant must work as hard with each successive breath as it did with the first. | ||
| + | |||
| + | The problem of STIFF atelectatic lungs is compounded by the SOFT thoracic wall that is pulled in as the diaphragm descends. Progressive atelectasis and reduced lung compliance then lead to a worsening clinical course.</spoiler> | ||
| + | * <spoiler text="What makes up the red hyaline material seen in HMD?">With a deficiency of surfactant, the alveoli collapse with each breath resulting in injury to the epithelial cells lining the alveolar wall. This injury causes a protein-rich, fibrin-rich exudate to be released into the alveolar spaces. This exudate forms the hyaline membranes. | ||
| + | |||
| + | The fibrin-hyaline membranes constitute a barrier to gas exchange, leading to carbon dioxide retention and hypoxemia. The hypoxemia itself further impairs surfactant synthesis leading to more lung damage.</spoiler> | ||
| + | |||
| + | == Additional Resources == | ||
| + | === Reference === | ||
| + | * [http://emedicine.medscape.com/article/976034-overview eMedicine Medical Library: Respiratory Distress Syndrome] | ||
| + | * [http://www.merckmanuals.com/professional/pediatrics/respiratory_disorders_in_neonates_infants_and_young_children/respiratory_distress_syndrome.html Merck Manual: Respiratory Distress Syndrome] | ||
| + | |||
| + | === Journal Articles === | ||
| + | * Clark RH, Gerstmann DR, Jobe AH, Moffitt ST, Slutsky AS, Yoder BA. [http://www.ncbi.nlm.nih.gov/pubmed/11598592 Lung injury in neonates: causes, strategies for prevention, and long-term consequences]. ''J Pediatr'' 2001 Oct;139(4):478-86. | ||
| + | |||
| + | === Images === | ||
| + | * [{{SERVER}}/library/index.php?/tags/48-hyaline_membrane_disease PEIR Digital Library: Hyaline Membrane Disease Images] | ||
| + | * [http://library.med.utah.edu/WebPath/PEDHTML/PEDIDX.html WebPath: Pediatric-Perinatal Pathology] | ||
{{IPLab 13}} | {{IPLab 13}} | ||
[[Category: IPLab:Lab 13]] | [[Category: IPLab:Lab 13]] | ||
Latest revision as of 16:45, 3 January 2014
Contents
Clinical Summary[edit]
This 28-hour-old white male was the product of an uncomplicated vaginal delivery by a G1 24-year-old mother whose pregnancy had also been uncomplicated. The infant was born pre-term at 36 weeks gestation and was appropriate for gestational age, weighing 2550 grams. Three hours after birth, the infant developed cyanosis and required 40% oxygen to maintain a pink color. Because of a worsening respiratory distress syndrome, the infant (1 day old) was transferred to a tertiary care hospital with a neonatal intensive care unit. Following the transfer, the respiratory distress progressed and the admitting arterial blood gases were pH 7.31, PaCO2 35, and PaO2 35. The condition of the patient continued to deteriorate despite therapy, and he became "shocky" with efforts to increase blood volume. He developed a persistent bradycardia and died about 4 hours after admission.
Autopsy Findings[edit]
The organs generally showed no abnormalities other than those of immaturity expected at this gestational age. There was moderate diffuse subarachnoid hemorrhage and a small amount of blood in the pleural and pericardial cavities.
Images[edit]
Virtual Microscopy[edit]
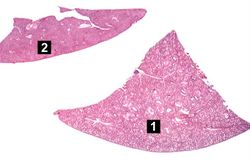
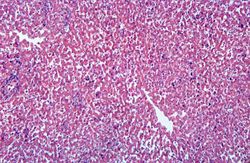
Liver[edit]
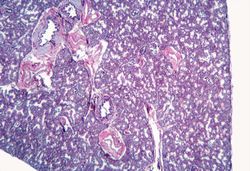
Lung[edit]
Study Questions[edit]
Additional Resources[edit]
Reference[edit]
- eMedicine Medical Library: Respiratory Distress Syndrome
- Merck Manual: Respiratory Distress Syndrome
Journal Articles[edit]
- Clark RH, Gerstmann DR, Jobe AH, Moffitt ST, Slutsky AS, Yoder BA. Lung injury in neonates: causes, strategies for prevention, and long-term consequences. J Pediatr 2001 Oct;139(4):478-86.
Images[edit]
| |||||
Births occurring at 38 to 42 weeks of gestation are considered term pregnancies. Anytime earlier are considered pre-term.
Appropriate for gestational age (AGA) is a term which means that an infant's weight and height were appropriate when adjusted for the gestational age of the child. Large for gestational age (LGA) and small for gestational age (SGA) are the alternative designations.
The normal weight for a child of this gestational age would be 2250 to 3000 grams.
Cyanosis is a bluish discoloration of the skin and mucous membranes resulting from increased concentrations of reduced hemoglobin in the blood. Cyanosis occurs when the blood oxygen saturation falls below 85%.
Respiratory distress syndrome (or hyaline membrane disease) is a common complication of prematurity, though it can also be seen in term births. The syndrome results from the functional immaturity of the neonatal lung. The syndrome usually presents within one hour of birth and is initially exhibited clinically by rapid respirations, grunting, and substernal retractions.
A normal pH for a child this age would be 7.37.
A normal PaCO2 level for a child this age would be 33.
A normal PaO2 level for a child this age would be 90.
Bradycardia is defined as a heart rate below 60 beats per minute. A normal heart rate for a neonate is 100 to 160 beats per minute.
Atelectasis is the collapse of an airway and lung, regardless of the cause, resulting in reduced or absent gas exchange.