Difference between revisions of "IPLab:Lab 3:Acute Myocardial Infarction"
Seung Park (talk | contribs) |
(→Virtual Microscopy) |
||
| (8 intermediate revisions by 2 users not shown) | |||
| Line 4: | Line 4: | ||
# Aspartate Aminotransferase (AST) 60 IU/L. | # Aspartate Aminotransferase (AST) 60 IU/L. | ||
# Total Creatine Phosphokinase (CPK) 165 IU/L. All of the activity was due to CPK III (MM) isoenzyme fraction; no CPK (MB) activity was detectable. | # Total Creatine Phosphokinase (CPK) 165 IU/L. All of the activity was due to CPK III (MM) isoenzyme fraction; no CPK (MB) activity was detectable. | ||
| − | # | + | # Troponin I 38 µg/L. |
== Autopsy Findings == | == Autopsy Findings == | ||
| Line 19: | Line 19: | ||
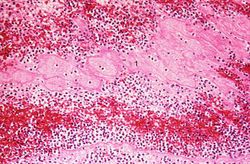
File:IPLab3AcuteMyocardialInfarction7.jpg|This is a photomicrograph of the lines of Zahn. Pale areas (1) represent platelets with some fibrin and the darker lines (2) represent RBCs and leukocytes enmeshed in fibrin strands. | File:IPLab3AcuteMyocardialInfarction7.jpg|This is a photomicrograph of the lines of Zahn. Pale areas (1) represent platelets with some fibrin and the darker lines (2) represent RBCs and leukocytes enmeshed in fibrin strands. | ||
</gallery> | </gallery> | ||
| + | |||
| + | == Virtual Microscopy == | ||
| + | === Heart: Acute Myocardial Infarction === | ||
| + | <peir-vm>IPLab3AcuteMyocardialInfarction</peir-vm> | ||
| + | |||
| + | === Normal Heart === | ||
| + | <peir-vm>IPLab2Hypertrophy_normal_Heart</peir-vm> | ||
| + | |||
| + | == Study Questions == | ||
| + | * <spoiler text="Are the serum enzyme results consistent with the time course of this clinical history?">The infarct occurred approximately 4 days prior to death. His CPK-MB levels would be expected to have gone down by now. His AST is slightly elevated and his LDH is moderately elevated with a high LDH1:LDH2 ratio. These findings are consistent with the clinical history.</spoiler> | ||
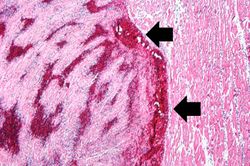
| + | * <spoiler text="Why do mural thrombi often form in infarcted hearts?">The endocardium is usually the most severely damaged after an arterial occlusion since it is at the end of the circulation of the heart. Thus, with the infarcted tissue in the endocardium there is an acute inflammatory reaction which initiates coagulation and thrombus formation.</spoiler> | ||
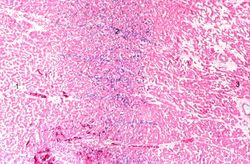
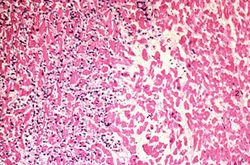
| + | * <spoiler text="What is the primary cell type in this inflammatory reaction?">At this stage it is primarily neutrophils, but there area a few macrophages. Usually, neutrophils enter an infarct by 12-24 hours and macrophages enter the lesion by 72 hours post-MI. By 3-7 days the lesion is primarily macrophages and by 10 days there are macrophages, fibroblasts, and endothelial cells (granulation tissue). The healing reaction in this patient may have been slower than normal because of his poor condition.</spoiler> | ||
| + | |||
| + | == Additional Resources == | ||
| + | === Reference === | ||
| + | * [http://emedicine.medscape.com/article/155919-overview eMedicine Medical Library: Myocardial Infarction] | ||
| + | * [http://www.merckmanuals.com/professional/cardiovascular_disorders/coronary_artery_disease/acute_coronary_syndromes_acs.html Merck Manual: Acute Coronary Syndromes] | ||
| + | |||
| + | === Journal Articles === | ||
| + | * Helft G, Worthley SG. [http://www.ncbi.nlm.nih.gov/pubmed/16352041 Anti-thrombotic, anti-platelet and fibrinolytic therapy: current management of acute myocardial infarction]. ''Heart Lung Circ'' 2001;10(2):68-74. | ||
| + | |||
| + | === Images === | ||
| + | * [{{SERVER}}/library/index.php?/tags/43-myocardial_infarct PEIR Digital Library: Myocardial Infarct Images] | ||
| + | * [http://library.med.utah.edu/WebPath/CVHTML/CVIDX.html WebPath: Cardiovascular Pathology] | ||
| + | |||
| + | == Related IPLab Cases == | ||
| + | * [[IPLab:Lab 1:Myocardial Infarction|Lab 1: Heart: Myocardial Infarction (Coagulative Necrosis)]] | ||
| + | * [[IPLab:Lab 3:Healed Myocardial Infarction|Lab 3: Heart: Healed Myocardial Infarction]] | ||
| + | * [[IPLab:Lab 4:Mural Thrombus|Lab 4: Heart: Mural Thrombus]] | ||
| + | * [[IPLab:Lab 4:Thrombosis|Lab 4: Coronary Artery: Thrombosis]] | ||
| + | * [[IPLab:Lab 4:Pulmonary Congestion and Edema|Lab 4: Lung: Pulmonary Congestion and Edema]] | ||
{{IPLab 3}} | {{IPLab 3}} | ||
[[Category: IPLab:Lab 3]] | [[Category: IPLab:Lab 3]] | ||
Latest revision as of 19:45, 17 September 2015
Contents
Clinical Summary[edit]
This 78-year-old male experienced a posterior myocardial infarction six years prior to this admission. Recently, he had begun to experience occasional angina. Four days prior to death, he experienced anterior chest pain and discomfort which he regarded as not too distressing. However, EKGs showed a classic acute anterior myocardial infarction in addition to the healed posterior infarct. The patient progressively deteriorated with left ventricular failure and died with arrhythmias and pulmonary edema. Pertinent laboratory data are:
- Aspartate Aminotransferase (AST) 60 IU/L.
- Total Creatine Phosphokinase (CPK) 165 IU/L. All of the activity was due to CPK III (MM) isoenzyme fraction; no CPK (MB) activity was detectable.
- Troponin I 38 µg/L.
Autopsy Findings[edit]
Examination of the heart showed a healed posterior infarct. The right coronary artery was completely occluded but partially recanalized. The left main coronary artery had severe atherosclerotic stenosis and a thrombus filling the lumen. The entire anterolateral aspect of the left ventricle was soft with variegated areas appearing hyperemic or pale. There was extensive mural thrombosis and reactive pericarditis.
Images[edit]
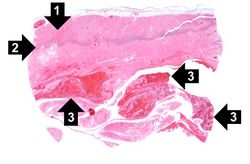
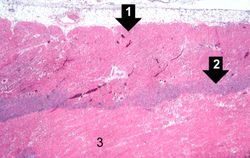
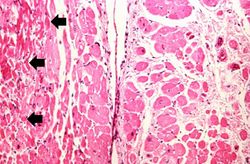
This is a low-power photomicrograph of infarcted heart. There is a layer of surviving myocardial tissue (1) along the epicardium and then a blue line (2) which represents the accumulation of inflammatory cells at the border of the infarct. There is thrombotic material (3) adherent to the endocardial surface.
Virtual Microscopy[edit]
Heart: Acute Myocardial Infarction[edit]
Normal Heart[edit]
Study Questions[edit]
Additional Resources[edit]
Reference[edit]
Journal Articles[edit]
- Helft G, Worthley SG. Anti-thrombotic, anti-platelet and fibrinolytic therapy: current management of acute myocardial infarction. Heart Lung Circ 2001;10(2):68-74.
Images[edit]
Related IPLab Cases[edit]
- Lab 1: Heart: Myocardial Infarction (Coagulative Necrosis)
- Lab 3: Heart: Healed Myocardial Infarction
- Lab 4: Heart: Mural Thrombus
- Lab 4: Coronary Artery: Thrombosis
- Lab 4: Lung: Pulmonary Congestion and Edema
Myocardial infarction is necrosis of myocardial tissue which occurs as a result of a deprivation of blood supply, and thus oxygen, to the heart tissue. Blockage of blood supply to the myocardium is caused by occlusion of a coronary artery.
Angina pectoris is chest pain produced by myocardial ischemia, it worsens upon exertion.
Arrhythmias are abnormal heart rhythms.
Pulmonary edema refers to the accumulation of fluid in the pulmonary alveolar and tissue spaces as a result of changes in capillary permeability and/or increases in capillary hydrostatic pressure.
AST is a NON-SPECIFIC marker of myocardial infarction (i.e., it is also elevated in other conditions, such as liver disease and skeletal muscle injury). AST levels peak at 48--72 hours following the infarction. A normal AST level would be less than 37 IU/L.
An elevated total CPK (a collective measure of all CPK isoenzymes) is a NONSPECIFIC marker for myocardial infarction. However, an elevation in the level of CPK-MB isoenzyme is a more specific marker for myocardial infarction. The CPK-MM isoenzyme is specific for skeletal muscle. CPK levels begin to rise 4-8 hours following an infarction, usually peak within the first 24-48 hours, and then return to baseline within 3-4 days. A normal CPK level is 35 to 250 IU/L.
Troponin I is a muscle contractile protein that is increased in serum after myocardial necrosis, it is a sensitive and specific marker of acute MI, and better than CK-MB as a cardiac injury marker. Normally troponin I values are less than 10 µg/L but values can rise 5 to 50 times after an acute myocardial infarction.
Recanalization is the process of the forming of channels through an organized thrombus so that blood flow is restored.
A thrombus is a solid mass resulting from the aggregation of blood constituents within the vascular system.
Mural thrombosis is the formation of multiple thrombi along an injured endocardial wall.
Pericarditis is inflammation of the pericardium - often with deposition of fibrin.
Mural thrombosis is the formation of multiple thrombi along an injured endocardial wall.
An occlusion is a blockage.