Difference between revisions of "IPLab:Lab 4:Thromboembolus"
Seung Park (talk | contribs) |
Seung Park (talk | contribs) |
||
| Line 25: | Line 25: | ||
* <spoiler text="What are the clinical sequelae of pulmonary thromboemboli?">Most (60-80%) pulmonary thromboemboli are clinically silent. In the remainder of the cases, pulmonary thromboemboli can cause sudden death, acute or chronic cor pulmonale, infarction, or hemorrhage.</spoiler> | * <spoiler text="What are the clinical sequelae of pulmonary thromboemboli?">Most (60-80%) pulmonary thromboemboli are clinically silent. In the remainder of the cases, pulmonary thromboemboli can cause sudden death, acute or chronic cor pulmonale, infarction, or hemorrhage.</spoiler> | ||
* <spoiler text="What is a paradoxical embolism?">When a venous embolus passes through an interatrial or interventricular septal defect and enters the systemic circulation.</spoiler> | * <spoiler text="What is a paradoxical embolism?">When a venous embolus passes through an interatrial or interventricular septal defect and enters the systemic circulation.</spoiler> | ||
| + | |||
| + | == Additional Resources == | ||
| + | === Reference === | ||
| + | * [http://emedicine.medscape.com/article/300901-overview eMedicine Medical Library: Pulmonary Embolism] | ||
| + | * [http://emedicine.medscape.com/article/1911303-overview eMedicine Medical Library: Deep Venous Thrombosis] | ||
| + | * [http://emedicine.medscape.com/article/1950759-overview eMedicine Medical Library: Noncoronary Atherosclerosis] | ||
| + | * [http://www.merckmanuals.com/professional/hematology_and_oncology/thrombotic_disorders/overview_of_thrombotic_disorders.html Merck Manual: Thrombotic Disorders] | ||
| + | * [http://www.merckmanuals.com/professional/pulmonary_disorders/pulmonary_embolism/pulmonary_embolism.html Merck Manual: Pulmonary Embolism] | ||
| + | * [http://www.merckmanuals.com/professional/cardiovascular_disorders/peripheral_venous_disorders/deep_venous_thrombosis_dvt.html Merck Manual: Deep Venous Thrombosis] | ||
| + | |||
| + | === Journal Articles === | ||
| + | * Garg K. [http://www.ncbi.nlm.nih.gov/pubmed/11813814 CT of pulmonary thromboembolic disease]. ''Radiol Clin North Am'' 2002 Jan;40(1):111-22, ix. | ||
| + | |||
| + | === Images === | ||
| + | * [http://peir.path.uab.edu/library/index.php?/tags/28-thromboembolus PEIR Digital Library: Thromboembolus Images] | ||
| + | * [http://library.med.utah.edu/WebPath/LUNGHTML/LUNGIDX.html#7 WebPath: Pulmonary Pathology] | ||
| + | |||
| + | == Related IPLab Cases == | ||
| + | * [[IPLab:Lab 4:Pulmonary Congestion and Edema|Lab 4: Lung: Pulmonary Congestion and Edema]] | ||
{{IPLab 4}} | {{IPLab 4}} | ||
[[Category: IPLab:Lab 4]] | [[Category: IPLab:Lab 4]] | ||
Revision as of 03:14, 22 August 2013
Contents
Clinical Summary[edit]
This 67-year-old male was hospitalized because of extensive atherosclerotic cardiovascular disease. Following surgery, during which diseased portions of the femoral arteries were bypassed, he developed massive pulmonary embolization and expired.
Autopsy Findings[edit]
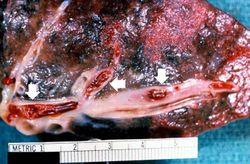
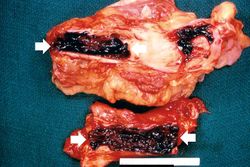
At autopsy, thrombi were found in the femoral and iliac veins, as well as in the larger pulmonary arteries.
Images[edit]
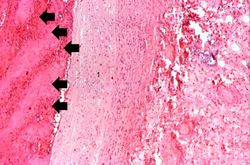
This is a photomicrograph of the wall of the pulmonary artery (1) containing the thromboembolus. In this case the artery wall looks normal. If this was a thrombus instead of a thromboembolus, you would expect to see some damage in the artery wall that would have initiated the thrombus. Note the lines of Zahn in the thromboembolus (arrows).
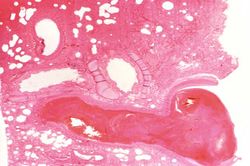
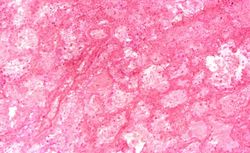
This is a low-power photomicrograph of the infarcted lung. The tissue is congested and has a very bland appearance due to coagulation necrosis of the lung parenchyma. You can still see the outlines of the alveoli and the cells that make-up the alveoli but there is almost complete loss of nuclei throughout this section.
This is a gross photograph of an infarcted testis. Because of the anatomy of the blood supply to the testis, torsion or the blood vessels often leads to venous occlusion (due to compression of the thin walled veins) but not arterial occlusion. Thus, blood still flows into the testis but it can’t get out! This leads to hypoxia and eventually to hemorrhagic necrosis.
This is a gross photograph of an opened abdomen at autopsy demonstrating loops of infarcted bowel (arrow). Vascular occlusion can lead to ischemic necrosis of the bowel. In this case, a section of bowel herniated through a fibrous connective tissue band and was strangulated, leading to ischemic necrosis.
This is a gross photograph of the fibrous band between the uterus and adjacent tissues. This fibrous scar tissue is probably left over from a previous surgery or an infection. A loop of bowel herniated through the opening produced by this fibrous band and became incarcerated leading to the ischemic necrosis seen in the previous image.
Study Questions[edit]
Additional Resources[edit]
Reference[edit]
- eMedicine Medical Library: Pulmonary Embolism
- eMedicine Medical Library: Deep Venous Thrombosis
- eMedicine Medical Library: Noncoronary Atherosclerosis
- Merck Manual: Thrombotic Disorders
- Merck Manual: Pulmonary Embolism
- Merck Manual: Deep Venous Thrombosis
Journal Articles[edit]
- Garg K. CT of pulmonary thromboembolic disease. Radiol Clin North Am 2002 Jan;40(1):111-22, ix.
Images[edit]
Related IPLab Cases[edit]
| |||||
A thrombus is a solid mass resulting from the aggregation of blood constituents within the vascular system.
An occlusion is a blockage.