Difference between revisions of "Histologic:Chapter 15"
(→Slide 117, Kidney (Masson)) |
(→Slide 118, Kidney (PASH)) |
||
| Line 47: | Line 47: | ||
=== Slide 118, Kidney (PASH) === | === Slide 118, Kidney (PASH) === | ||
| − | + | [[File:HistologicChapter15Glomerulus.jpg|thumb|200px|Glomerulus]] | |
The renal corpuscles on Slide 118, Kidney (PASH) are to be studied in detail. | The renal corpuscles on Slide 118, Kidney (PASH) are to be studied in detail. | ||
Revision as of 05:41, 18 July 2014
Contents
Kidney[edit]
A good knowledge of normal kidney histology is essential for the understanding of various diseases of the kidney.
Slide 117, Kidney (Masson)[edit]
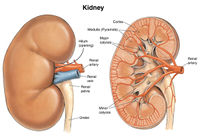
Observe Slide 117, kidney (Masson) with the unaided eye to distinguish the lighter stained medulla from the more peripheral and darker-staining cortex. Now, with low and medium powers of the microscope identify:
- The thin, fibrous capsule of the kidney. Scan the entire slide to observe that the only prominent connective tissue fibers within the kidney are in association with blood vessels.
- The cortex containing the renal corpuscles.
- The medulla in which renal corpuscles are lacking.
- The larger blood vessels at the corticomedullary junction. These are arcuate arteries and veins.
Study the cortex of the kidney for details of its organization. On Slide 114, Slide 116, Slide 117, and Slide 118 identify:
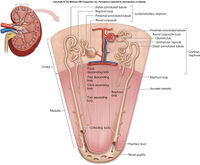
Pars radiata (medullary rays) are columns of straight tubules extending from the cortex into the medulla and from the medulla into the cortex.
The straight segments of the proximal and distal tubules and the straight collecting tubules are located here.
Pars convoluta (cortical labyrinths) areas occupy the region between pars radiata.
Within the pars convoluta can be found renal corpuscles, proximal convoluted tubules (PCT), distal convoluted tubules (DCT), and blood vessels (the interlobular arteries and veins and the afferent and efferent arterioles). A kidney lobule consists of a pars radiata and “half” of each adjoining pars convoluta.
Learn to distinguish the PCT from the DCT. With the light microscope the straight portion of the proximal tubule is histologically similar to the PCT and the straight portion of the distal tubule is similar to the DCT.
Proximal convoluted tubule (PCT). The PCT may be up to 14 mm in length. This is more than twice as long as the average DCT, which is about 5 mm long. Thus, one sees more sections through PCT in any given region of the pars convoluta than through DCT.
- The PCT stains darker than the DCT.
- The PCT cells are larger and the cytoplasm is more granular than the cells of the DCT. This is due to the large number of mitochondria in the cytoplasm of the PCT cells.
- The cell boundaries of the PCT are less distinct than the DCT because the membranes of the PCT cells are more highly interdigitated with the membranes of neighboring cells. And the PCT is larger in cross section than the DCT.
- The apical surface of the PCT exhibits microvilli, about 1.2 μm in length, which form a brush border when observed with the light microscope. This border disintegrates quickly when postmortem changes set in. A brush border is lacking on cells of the DCT although the EM demonstrates the presence of a few microvilli.
- The cells of the PCT are low columnar to pyramidal; those of the DCT are more cuboidal in shape.
Slide 114, Kidney[edit]
Slide 116, Kidney[edit]
Slide 118, Kidney (PASH)[edit]
The renal corpuscles on Slide 118, Kidney (PASH) are to be studied in detail.
First, with low power, become oriented to the section on Slide 118. This is a tangential section through the cortex of the kidney. Thus, renal corpuscles are found throughout the. Note that tubules in the pars radiata are cut in cross section and appear to be grouped into bundles surrounded (or bordered) by pars convoluta. We will study these tubules in detail later.
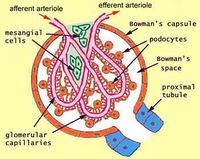
On high power study several renal corpuscles on Slide 118. A renal corpuscle ranges from 150 to 250 μm in diameter. It consists of a tuft of capillaries called the glomerulus and a surrounding epithelial capsule called the glomerular capsule (Bowman’s capsule). This latter structure has an outer layer of simple squamous epithelial cells with a basement membrane. The cells and basement membrane form the parietal layer of Bowman’s capsule, which surrounds Bowman’s space or the urinary space. A layer of visceral epithelial cells covers the glomerular basement membrane. The cells of this highly modified epithelial layer are called podocytes because of numerous foot-like processes (pedicels) that they possess. The space between the visceral and parietal layers of Bowman’s capsule is termed Bowman’s space or urinary space within which the glomerular filtrate is collected and passes into the PCT. The parietal epithelial cells are continuous with the neck of the PCT and with the visceral layer at the vascular pole.
Identify:
- The simple squamous epithelial cells of the parietal layer.
- The basement membrane on which the cells lie.
- The urinary space.
The glomerulus is a specialized bed of capillaries connecting an afferent arteriole with an efferent arteriole at the vascular pole of the renal corpuscle. The urinary pole of the renal corpuscle where the glomerular filtrate passes into the PCT usually lies opposite the vascular pole.
Find, if present, a renal corpuscle sectioned so as to demonstrate both the vascular and urinary poles.
Study several glomeruli in detail.
- A glomerulus appears lobulated since the looped capillaries from a major capillary branch are grouped together. About 5-8 major capillary trunks (lobules) are formed in each glomerulus. Up to 50 capillary loops may be present.
- Anastomoses occur between capillaries of the same lobule and of different lobules.
- The afferent arteriole supplying blood to the glomerulus is usually larger than the efferent arteriole.
- The endothelial cells lining the capillary lumen are fairly large, attenuated, flattened cells with nuclei bulging into the lumen. The fenestrated endothelium has numerous pores that vary from 50 to 100 nm in diameters. These endothelial cells are only partially surrounded by a basement membrane that is about 300 nm thick in adults. The capillaries of each lobule wind around a common axis that appears as a cellular stalk of mesangial cells and mesangial matrix. Basement membrane is lacking between the capillary endothelium and the stalk of the capillary lobule occupied by the mesangial cells and mesangial matrix. Hence, instead of surrounding the entire lumen of a capillary loop, the basement membrane is reflected onto adjacent capillary loops. The mesangial cells are located inside of the basement membrane of the capillary lobule, and they are in direct contact with the endothelial cells where basement membrane material is lacking.
- Identify the nuclei of endothelial cells, mesangial cells lying in mesangial matrix, and the nuclei of podocytes.
On Slide 118 select, an “open appearing” capillary loop cut in cross section, lying towards the outer edge of a glomerulus and within which a nucleus can be seen bulging into the lumen. This is the nucleus of an endothelial cell. The nuclei tend to lie on the wall of the capillary loop nearest the central axis.
Find a slightly darker staining nucleus, about the same size as the endothelial nucleus, embedded in the denser, darkly stained PAS-positive material. This is a mesangial cell nucleus and the PAS-positive staining material is mesangial matrix. The mesangial cell lies to the inner side of the basement membrane. Electron micrographs show that the mesangial cells are in direct contact with the endothelial cells. The mesangial matrix produced by the mesangial cells is a basement membrane-like material that increases with age and in certain disease states such as diabetic nephropathy and glomerulonephritis.
Identify slightly larger, slightly paler staining nuclei lying outside the basement membrane. They are podocyte nuclei. The interdigitated cytoplasmic extensions of the podocytes, which line the outside of the basement membrane, can be seen only with the electron microscope.
Filtration Barrier. In order for substances in the blood to reach the urinary space as glomerular filtrate they must pass through the filtration barrier. This important barrier includes the endothelium of the capillary, basal lamina and slit pores between adjacent pedicles (foot processes) of the podocytes. The slit pores are about 250 nm in diameter and they are bridges by a thin diaphragm called the filtration slit membrane.
Identify on Slide 117 the endothelial cells of the glomerular capillary, the mesangial cells and mesangial matrix, and the podocytes. On this section stained with Masson’s stain the basement membrane of the glomerulus appears as a very thin blue line. The mesangial matrix is readily identified as the purplish-staining material between capillaries.
Juxtaglomerular apparatus. On Slide 118 attempt to find a juxtaglomerular apparatus where the distal tubule comes into close association with the afferent glomerular arteriole at the vascular pole of each Bowman’s capsule. This composite structure consists of the macula densa of the distal tubule, lacis cells (extraglomerular mesangial cells) and juxtaglomerular cells (JG cells). The latter cells are modified smooth muscle cells in the tunica media of the afferent arteriole. These secretory, epithelioid cells replace the smooth muscle cells of the media only in the localized region of the juxtaglomerular apparatus. The JG cells are separated from the cells forming the macula densa only by a basal lamina. The JG cells are important since they secrete renin.
The macula densa is identified as being an area of tall, slender cells on the side of the distal tubule adjacent to the afferent arteriole. Since the cells are narrow, the nuclei appear closely packed together, and with the light microscope the area appears denser than surrounding areas (macula densa = “dense spot”). The function of these cells is to monitor sodium in the distal tubule and “pass” this information to the JG cells to alter their secretory activity.
The lacis cells are small agranular cells lying in a triangular area bounded by the afferent and efferent arterioles and the macula densa. The lacis cells are embedded in a dense network of basement membranes. They are continuous with the mesangium of the capillary stalk. The specific function of lacis cells is not well understood, although it has been associated with the secretion of erythropoietin.
Study the tubules in the medulla of the kidney on Slides 114, 116, and 117. A straight collecting tubule lying in the pars radiata of the cortex receives 7 to 10 arched collecting tubules as it passes into the outer zone of the medulla. Continuing into the inner zone of the medulla the straight collecting tubules unite with other similar tubules to form large papillary ducts. These open into the minor calyces at the area cribrosa of a renal papilla. Papillary ducts are not found in the outer zone of the medulla. The straight collecting tubules have a diameter of about 40μm as compared with a diameter of 200 μm for the papillary ducts.
On Slide 117 identify straight collecting tubules in the medulla. They exhibit a lining of large pale staining, simple columnar cells with well-defined cell boundaries.
Identify the smallest tubules cut in cross section in the medulla. These are the thin segments of the loops of Henle. Only the juxtamedullary nephrons have thin segments extending deep into the medulla. The thin segments of Henle’s loop are easily confused with capillaries or venules. They are composed of a single layer of flattened epithelial cells having round to ovoid nuclei that tend to bulge into the lumen. The cells sit on a basement membrane. The overall diameter of the segment is about 15μm, and cross sections of them usually contain 3 to 5 nuclei. Remember that the loops of Henle are made up of both thick and thin segments. The thick segments form descending and ascending limbs. An abrupt change occurs in the epithelium where the thick segments meet the thin segments.
Return to Slide 118 and identify the collecting ducts in the pars radiata. They have many nuclei in cross section and have distinctly visible cell boundaries. In the pars convoluta the proximal convoluted tubules are easily identified by the PAS-positive staining of their brush border. The straight portion of the proximal tubule in the pars radiata appears similar. The straight portions of the distal tubules (thick ascending segment of Henle’s loop) located in the pars radiata appear to have undergone more postmortem change than other parts of the tubule. The straight distal tubules exhibit cells that are somewhat disrupted and pulled free of the basement membrane. Many cells appear to be “floating” within the lumen of the tubule. Identify the straight proximal and distal tubule.
Blood supply
The circulation of blood through the kidney is rather complex and should be studied in your textbook before attempting to understand it from slides. Only a few aspects of the overall circulation can be seen on any one microscopic slide.
On Slide 117 identify the arcuate arteries and the arcuate veins at the corticomedullary junction. The arteries are continuations (branches) of the larger interlobar arteries.
Each arcuate artery gives off several interlobular arteries that pass perpendicularly through a pars convoluta to the surface of the kidney. Identify interlobular arteries on Slide 117; they are very small arteries or arterioles. Thin-walled interlobular veins (mostly venules) are seen adjacent to some of the interlobular arteries. The arteries and veins pass more or less through the middle of a pars convoluta. The area between two interlobular arteries and veins is a kidney lobule. On Slide 118 identify interlobular arteries cut in cross section and lying within a pars convoluta. A number of afferent glomerular arterioles are given off by the interlobular artery before it terminates as a capillary bed beneath the capsule of the kidney.
On Slide 117 identify the erythrocytes in capillaries that are interspersed between the convoluted tubules. In the outer cortex, the capillaries originate from the efferent arterioles to form a peritubular plexus, which in the living condition appears to bathe the tubules in blood. The capillaries drain into cortical venules that empty into interlobular veins that accompany the interlobular arteries.
The efferent arterioles leaving glomeruli near the medulla are relatively larger than the efferent arterioles in the outer cortex. They extend into the medulla as the arteriolae rectae spuriae. Pursuing a straight course in the medulla, these vessels give rise to capillary nets that extend deeply into the papillae. Veins called venae rectae return the blood to the arcuate veins. Collectively the blood supply of the medulla in which these thin-walled vessels make hairpin loops is called the vasa rectae.
Interstitial connective tissue. The connective tissue of the kidney is not nearly as extensive as in other organs. Most of the prominent connective tissue is in association with blood vessels, lymphatics and nerves. The more delicate and looser connective tissue spreads through the renal parenchyma. It is more abundant in the medulla than in the cortex. This poorly developed interstitial tissue consists principally of reticular and collagenous fibers with associated fibroblasts and macrophages. Observe on Slide 117 (Masson) that the large blood vessels are invested with the densest connective tissue, the adventitia. Very delicate collagen fibers can be seen surrounding tubules in the medulla. They appear as a pale blue network. Reticular fibers also form a diffuse network around the tubules. Compare the amount of interstitial connective tissue in the medulla with the amount present around the convoluted tubules of the cortex. The interstitial diseases of the kidney form from or directly affect the interstitial tissue. In severe systemic infections, non- specific inflammatory changes can occur in the interstitium.
The sinus of the kidney is the concave indentation or potential cavity on the hilus side of the kidney. It lies adjacent to kidney cortex of the renal columns and to medulla. It contains loose connective tissue and fat. In it are embedded branches of the renal artery and vein, lymphatics, nerves, minor calyces, major calyces and the renal pelvis.
Slide 92, Kidney, Ureter, Vessels[edit]
Study Slide 92. Section through the sinus of the kidney showing several blood vessels, nerves, and a section of ureter, all embedded in loose connective and adipose tissue (H&E).
Ureter and Urinary Bladder[edit]
Ureter[edit]
The ureters conduct urine from the kidneys to the bladder. They are about 12 inches long, course behind the peritoneum, and consist of three layers (a mucosa, a muscularis and a fibrosa).
Slide 120, Ureter (Masson)[edit]
Study Slide 120, Ureter (Masson), which is a cross section through the lower one-third of the ureter. At low and medium power observe:
The mucosa consisting of transitional epithelium and a lamina propria. Note the stellate-shaped lumen formed by the folds of the lamina propria, the density of the lamina propria, and the thickness of the epithelium.
The muscularis has three layers of smooth muscle since this section was taken from the lower one-third of the ureter. The upper two-thirds of the ureter has only two layers of smooth muscle in the muscularis. Identify, here, an inner longitudinal layer with fibers cut in cross section, the middle circular layer and an outer longitudinal layer. It is this outer layer that is the “extra layer” of the lower ureter. Note how the muscle bundles are separated by abundant connective tissue.
Identify the fibrosa lying outside the muscularis. This loose connective tissue layer binds the ureter to adjoining structures. Observe the blood vessels running through the fibrosa, which also contains nerves, lymphatics and fat cells.
Slide 119, Ureter (H&E)[edit]
Examine Slide 119, Ureter (H&E) under low and medium power for most of the features just studied on Slide 120. In addition, note that:
- With H&E, the muscle layers do not contrast well with the connective tissue fibers. Hence, it is difficult to distinguish that the middle portion of the ureter from which this section was taken has only two muscle layers instead of three. These are an inner longitudinal layer and an outer circular layer.
- Note the abundance of adipose tissue in the fibrosa. Identify the small arteries and veins occurring in this layer.
- Study the mucosa of slide 119 at high power.
It consists of a transitional epithelium of 5 to 6 cell layers thick. The surface cells of transitional epithelium, called cap cells, are larger and stain more darkly than the underlying cells. In some areas, the surface cells are stretched so as to appear almost squamous. The epithelium rests on a basement membrane, but the membrane is so thin that it is only identified with the electron microscope.
The lamina propria is a rather dense-appearing connective tissue layer between the epithelium and the muscularis. It contains collagenous fibers, elastic fibers and connective tissue cells. In the Masson-stained ureter, Slide 120, venules and capillaries are more readily seen within the lamina propria than they are in Slide 119.
Study the muscularis on Slide 119. This section is from the middle ureter that has only two layers of smooth muscle, an inner longitudinal and an outer circular layer. Contraction of the smooth muscle aids in passing the urine through the ureters.
Urinary Bladder[edit]
The urinary bladder consists of a mucosa, a muscularis and an adventitia that is either a fibrosa (where it blends with the connective tissue of surrounding structures) or a serosa (found only on the superior surface where the bladder is covered with peritoneum).
Slide 121, Urinary Bladder (H&E)[edit]
Scan the slide with low and medium powers to identify the three major layers.
Study the mucosa for details. A lining of transitional epithelium and underlying lamina propria form the mucosa. The empty bladder usually has a folded mucosa, the distended bladder a smooth one. Examine the epithelium in different regions of this section. In the relaxed bladder, as seen here, the epithelium is six or more cell layers thick; whereas in the distended bladder the epithelium is so stretched it appears to be only two or three cell layers thick. Recall that the epithelium is a special type of stratified epithelium that undergoes “transitional changes” to allow for the filling and emptying of the bladder.
Examine the surface cells. Observe in some regions their dome-shaped apices, and how they appear to “cap” the smaller underlying cells. These cap cells are occasionally binucleated. They are stretched into a “squamous” layer in the distended bladder. The cells immediately beneath the surface cells are pear-shaped or flask-shaped and their apices fit into facet-like indentations on the underside of the surface cells. The basal layer cells undergo mitosis to replenish the surface cells sloughed off into the lumen of the urinary bladder.
The luminal plasma membrane of the surface cells is thicker than most plasma membranes. This specialization, in conjunction with the superficial layer of cytoplasm containing numerous tonofilaments (microfilaments), serves to protect the epithelium from the hypertonicity of the urine, prevents urine resorption and acts as a barrier to the loss of water from the cells into the hypertonic urine.
The connective tissue underlying the transitional epithelium is the lamina propria. It is mostly collagenous fibers in which some elastic networks occur. Lymphocytes wander through the lamina propria and an occasional solitary lymphatic nodule can be present (but it is unlikely that you will see one on our slides). Observe that the deeper region of the lamina propria gives rise to an extensive capillary bed beneath the epithelium.
The muscularis of the bladder has three layers of smooth muscle indistinctly arranged into an inner longitudinal layer, a middle circular layer, and an outer longitudinal layer. The middle circular layer is the thickest but this may be difficult to identify on your slides, since the different muscle bundles tend to interlace and anastomose. Observe the abundant connective tissue that separates bundles of muscle. The muscularis has an abundant blood supply with an extensive capillary network.
Adventitia. This section of bladder is covered by a serosa consisting of a surface mesothelium.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
A normal alkaline phosphatase is 39 to 117 U/L.