Clinical Summary[edit]
This 68-year-old white female was afflicted with severe emphysema due to α1-antitrypsin deficiency. She had a 10 pack-year history of cigarette smoking but she had quit smoking 30 years ago. She elected to undergo lung volume reduction surgery to reduce complications of her emphysema. Post-operatively, she was ventilator dependent and her liver function declined. Further studies revealed hepatic cirrhosis. Her pulmonary function continued to decline and she died 26 days after her initial surgery.
Autopsy Findings[edit]
There were severe emphysematous changes in all lung lobes and there was massive hemorrhage throughout the lungs (combined lung weight: 3510 grams). The liver weighed 860 grams and there was micronodular cirrhosis.
This is a gross photograph of the lungs from this case. The rough friable material on the surface of the lung (arrows) is fibrinous exudate and fibrous tissue. This reaction on the surface of the lung is due to the recent surgery. The emphysematous changes are not easily appreciated in this photograph.
This is a gross photograph of the cut sections of lung from this case. The lung parenchyma is markedly hemorrhagic and consolidated. Again the hemorrhage makes it difficult to appreciate the emphysematous changes.
This is a gross photograph of the bronchi and lungs. Note the hemorrhage in the bronchi and in the lung parenchyma.
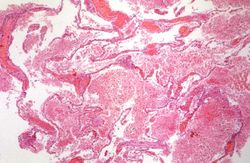
This low-power photomicrograph demonstrates the hemorrhage present throughout the lung. Note also the large air spaces; even though they are filled with blood, the emphysematous enlargement of the spaces is appreciable.
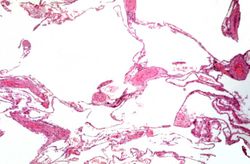
This is a low-power photomicrograph from an area of the lung without significant hemorrhage. The enlarged, emphysematous air spaces are easily appreciated.
This is a gross photograph of the liver from this case. The capsule is somewhat thickened and the surface is slightly roughened, though it is difficult to appreciate the nodularity of the liver.
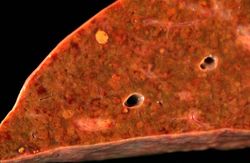
This is a gross photograph of the cut section of liver from this case. In this view the liver looks smaller than normal and there is a definite micronodular appearance.
This is a closer view of the cut section of liver from this case. There is a definite micronodular pattern to the liver parenchyma.
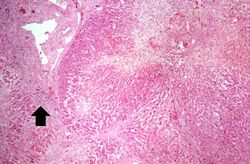
This is a low-power photomicrograph of an H&E-stained section of liver. There are increased numbers of inflammatory cells in the periportal region (arrow) and the central vein areas are pale.
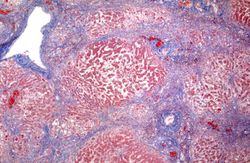
This is a low-power photomicrograph of a trichrome-stained section of liver. There is bridging fibrosis (blue material) between portal regions.
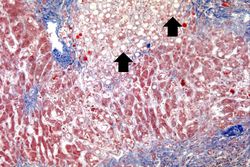
This is a higher-power photomicrograph of a trichrome-stained section of liver. This section demonstrates the fibrosis (blue material) and the fatty change (arrows).
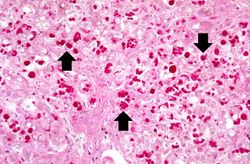
This is a high-power photomicrograph of liver stained with periodic-acid Schiff's (PAS) stain. This demonstrates the PAS-positive granules of defective α1-antitrypsin that accumulate in the Golgi of hepatocytes (arrows).
Study Questions[edit]
α1-antitrypsin deficiency is an autosomal recessive disorder caused by mutations in the protease inhibitor locus of chromosome 14. In the mutations that lead to a deficiency of the enzyme, the protein is transcribed but there is abnormal folding of the protein, thus it cannot be processed by the endoplasmic reticulum of hepatocytes. The protein, therefore, accumulates in the endoplasmic reticulum forming PAS-positive granules.
α1-antitrypsin is the major antiprotease and is responsible for inhibiting neutrophil elastase that can cause destruction of the alveolar wall. With α1-antitrypsin deficiency, neutrophil elastase goes unchecked and tissue damage ensues.
Smoking increases the numbers of neutrophils in the lung and accentuates the release of elastase from these neutrophils. With a deficiency of α1-antitrypsin there is marked tissue damage.
The abnormal α1-antitrypsin protein accumulates in hepatocytes of all patients with this abnormality but only 8 to 20% develop cirrhosis. The exact mechanism for hepatic cirrhosis in patients with α1-antitrypsin deficiency is not well understood.